Diastasis Recti - Part 2
What does it mean to “heal” or close a Diastasis?
Ah. I have so many feels for this question. Let me start by saying it is never too late to do something about your DR, if you want to do something about it.
Next - we need to unpack what it means to ‘heal’ a Diastasis Recti.
Unfortunately, the health and fitness industry sold you a false idea that you can ‘heal’ a DR. Healing implies that the connective tissue that breaks down in a DR can reconnect, and that is simply just not the case (without surgery - more on this below). So to heal a DR is not really a thing. BUT if when you say “heal” you mean 'control the gap’, ‘reducing coning or tenting’, ‘resolution of symptoms’, ‘improving performance’, or ‘getting back to the activities you used to do before baby’ - then the answer is YES - all of this is possible.
It should be noted that there isn’t a great definition for when a DR is resolved or ‘closed’ either, yet that term gets tossed around a lot. Because of our definition of Diastasis Recti (greater than 2-3 cm separation) a DR is considered closed when it no longer is beyond 2-3 cm.
Evidence does seem to show that exercise done prenatally and/or in postpartum may reduce DR (Khandale, 2016, Bernard 2014). But let it be known that reduction and prevention are two entirely different things. So when you see people claiming to be able to prevent DR with XYZ - not a thing. Remember DR happens in 100% of pregnant people. In other words it’s not preventable. Also, in the literature, there is no agreement for what specific movement or movements should be done to achieve this reduction or resolution of DR. There is a wide range of what is described as ‘exercise’ from study to study. Everything from ‘core exercise’, ‘TA training’ or even just walking is has been show to decrease DR. IMHO it makes sense that we can’t pin down a one size fits all remedy for DR. Here’s why…
As I mentioned above, one of the standard test used to evaluate DR is the sit up test. However, since it’s such a low threshold test, just because a person can pass the sit up test doesn’t mean they would be able to “pass” or manage pressure at the abdominal wall during a harder test like a hollow body hold. So does this mean they have closed their DR, or that they haven’t? Or maybe they have not ‘closed the gap’ of the DR but have firmed up the depth of the separation and have no signs of coning or doming? Which of these demonstrates resolution of DR? The answer is - the test that evaluations the function that is most closely related to that person’s goals. In other words - What functions does the individual person require to perform their activities of daily life and recreation? Once this is identified, this is what we should look at on an individual basis to determine DR status. This is because ‘closing’ a DR is a functional capacity. IMHO it matters less IF a DR is present… but rather can you manage pressure to control the gap to meet the needs of whatever it is you want to do?
For example - if I were Simon Biles, my core would need to function at an elite level to meet the demands of olympic gymnastics competition. Luckily I’m not Simone, so I only need a core that functions to manage pressure of my lifestyle which includes: lifting weights, yoga, running, carrying/lifting/bending, managing a 4 year old and a new baby etc. My core only has to be strong enough to manage pressure around my DR separation during these tasks. Does it mean I haven’t closed my DR if I can’t manage “Simon Biles level” pressure? Of course not. Also if we tested Simone Biles on “my level” she’d probably never be challenged - not an appropriate way to evaluate her.
We can improve DR with exercise prenatally and postpartum, but it’s probably not necessary for a majority of pregnant people. Studies show that a greater than a 2-3cm gap was found in 35-39% of people who were 6mo postpartum (Fernandes da Mota, 2015, Sperstad 2016). This means that more than 60% (give or take) of postnatal people in these studies had a natural reduction or resolution of their DR without any specific intervention designed to control, reduce or target the DR. This is good news! … It means that for the majority of you - there’s nothing you have to do to reduce your DR - if that’s is even something you care about doing.
For those of you who are looking to “close” your diastasis - that might not be a thing - it more likely will be a moving target based on your lifestyle, and activity levels. It is possible that with enough of a challenge you would always ‘fail’ a functional DR test at some point. And that’s ok…
Not fully resolving your DR might actually be a good thing… We actually might want to keep a DR around postpartum. There’s good reason for this: remember DR is a normally occurring adaptation to accommodate growing baby. If there might be any plans in your future for baby #2 you would want to maintain ability for this adaptation. Let this be another reminder for those of you (me) getting bombarded with gimmicky mechanisms (bands, belts, and exercises) saying DR can be completely cured - and to just keep scrolling.
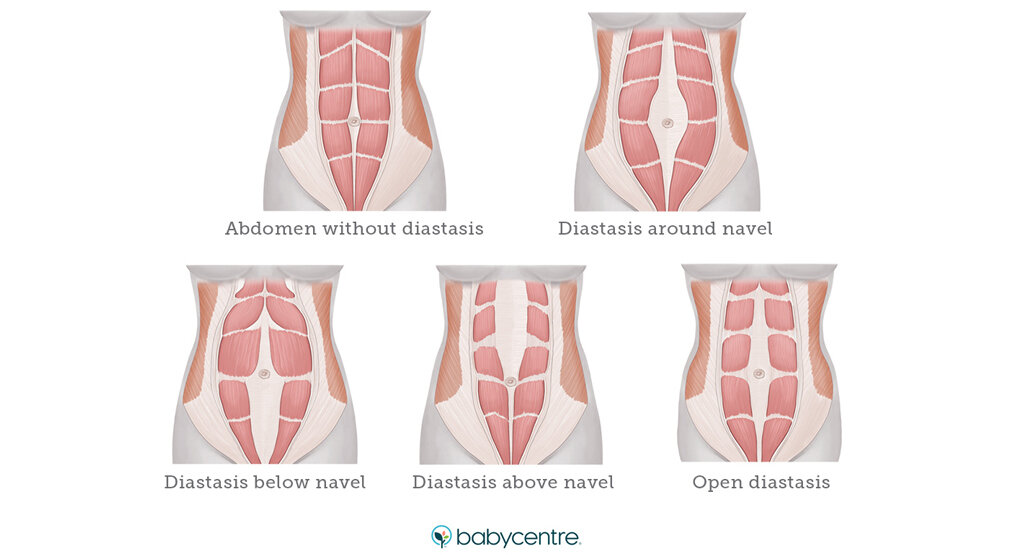
Image taken from babycenter.com
Why (else) might Diastasis Recti NOT matter?
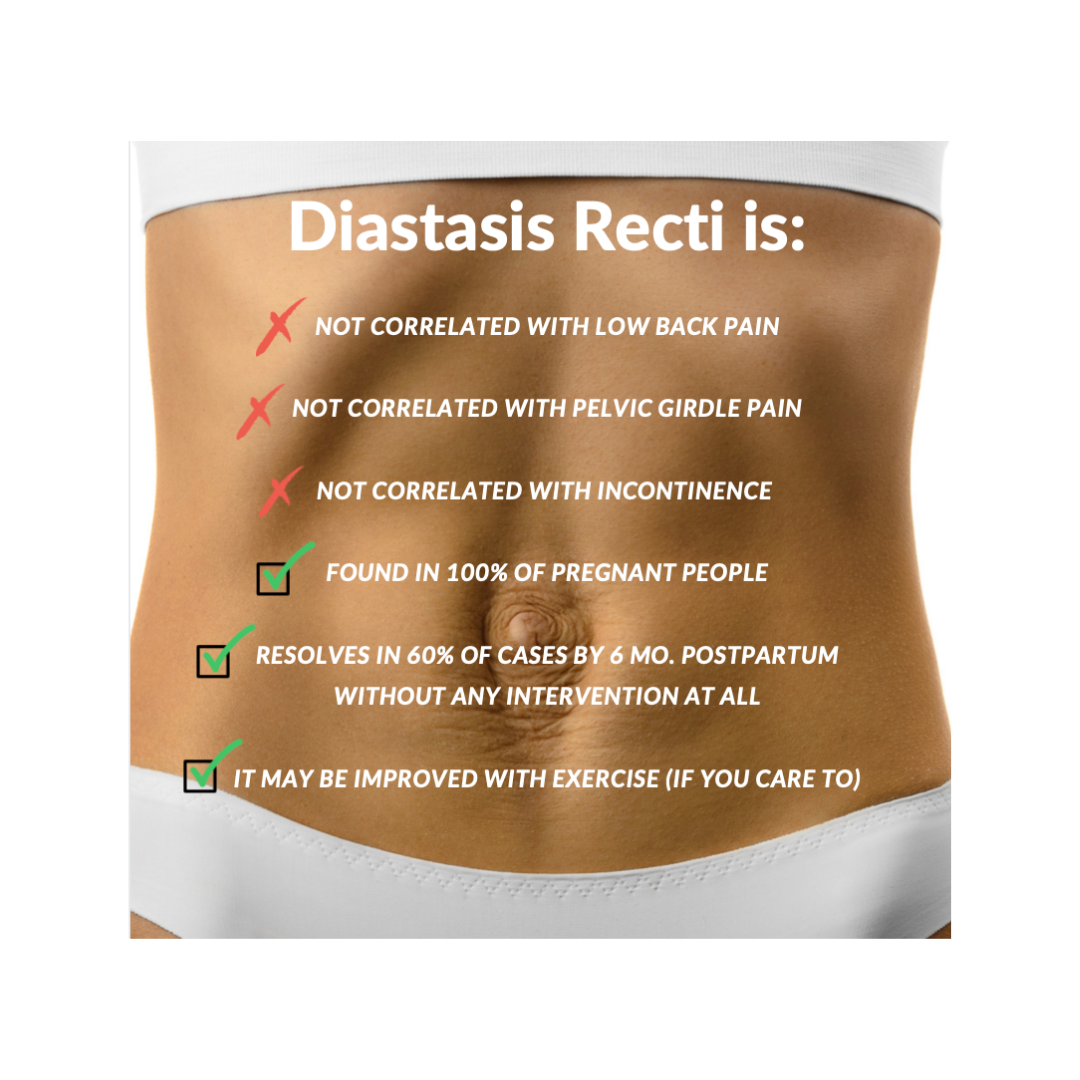
I’ll say it again - DR happens in 100% of pregnant people so therefore it’s not preventable. It is a normal, and dare I say, desirable adaptation in pregnancy!
On top of this, recent studies show that…
DR in postpartum people is NOT correlated with back pain. So if there is a DR, and it’s not correlated with pain - why are we so worried about it? (Gluppe 2021, Benjamin DR, 2019, Sperstad, 2016, Fernandez da Mota 2015)
DR in postpartum people is NOT correlated with pelvic girdle pain. So if there is a DR, and it’s not correlated with pelvic girdle pain - why are we so worried about it? (Gluppe 2021)
DR in postpartum people is NOT correlated with incontinence. So if there is a DR, and it’s not correlated with pain - why are we so worried about it? (Gluppe 2021, Fernandez da Mota 2015)
Weak evidence shows potential correlation with pelvic organ prolapse (POP) (Benjamin DR, 2019) - so the jury is out on this one.
THIS IS HUGE. And also flies in the face of 95% of the information that is put out there about Diastasis Recti to and for pregnant and postpartum people.
Have you ever seen a DR program being advertised with some (garbage) info about how “you better hurry and fix your DR because it’s related to pain and incontinence” at some point down the road?? I’ll answer for you - yes, all the damn time. Even some of the more reputable sources that I see out there tend to have poor wording around DR related to what this data is showing.
Summary of what we actually know about Diastasis Recti based on current research.
Why might DR matter?
If it’s not any more likely to be related to pain, or incontinence, what’s the big deal?
Recent studies show DR severity is correlated with poorer quality of life (Benjamin DR 2019).
I’m going to get a bit negative here, but there is a whole industry targeting the headspace of postpartum people. Societal pressures targeting the body image of birth people and females. Social media reinforcing these false ideals and focusing on aesthetics. If you’ve been there, (and maybe even if you haven’t) you know what I’m talking about… “Mummy tummy”, “mom pooch”, “FUPA”, “bounce back after baby”, “get your body back”, and more really targeted approaches to make us birthing people feel ‘less than’ or that we are lacking something integral because of the way our bodies look after baby. All of them selling us some sort of device or gimmick, band, belt, weight loss supplement, or ‘these 5 exercises to XYZ’ designed to vilify this totally normal condition, make you feel bad for having it, and fueling a false need to ‘fix it’.
Here’s some pictures of what DR is not… these show some of the things you will see out there being sold to pregnant people as DR along with a way to ‘fix’ it.
These are NOT pictures of Diastasis Recti, just a sampling of the DR related propaganda shared on social media targeting new parents.
You do not need to fix your Diastasis. You are perfect as you are.
Unless of course you want to. You may feel your DR is holding you back from a performance stand point or you may be someone who still feels motivated to ‘close’ your DR for aesthetic reasons, that is ok too. It is fine to want to have aesthetic goals for your body, I just challenge you to take a deeper dive on why you feel these feelings and what may or may not be driving them.
It also should be noted that in some cases, there is a risk that the functional integrity of the connective tissue at the linea alba would be compromised enough to result in issues like an umbilical hernia. This is rare, but in many cases can still be treated conservatively with physical rehab, and not require surgery. In other instances, surgery may be an option. Note - The surgery failure rate for umbilical hernia’s is suggested to be as much as 40% (Hickey, 2011), so even if you are a surgical candidate, learning how to support a surgical repair with exercises and physical therapy is highly recommended to ensure as much success here as possible.
What to do next?
If you are worried about your Diastasis Recti for any reason, it’s good to get evaluated by a professional. You’ll want to find someone who can properly evaluate your current capacity and goals to create an individualized program for your specific needs. When looking for help, Pelvic Health Physical Therapists are a great resource, not your OB or midwife. Your OB or midwife are experts on all things birth, but they don’t have nearly as good of an understanding of the musculoskeletal system necessary for giving individualized recommendations for DR. So if you do discuss DR with your OB or midwife, hopefully it’s just to get a proper referral. To find a certified PHPT in your area head to https://aptapelvichealth.org. Armed with the research mentioned above, you’ll be equipped with the tools to understand your evaluation, diagnosis, and ask some really good questions to make sure you get the right care for you.
If you’re in Massachusetts or local to Boston and interested in meeting with me to talk more about your specific situation as it relates to Diastasis Recti, pregnancy/postpartum, movement and exercise please follow the link below!
References
Aswini D, Srihari S K. An Overview of the Studies on Diastasis Recti Abdominis in Postpartum Women. J Gynecol Women’s Health. 2019: 14(5): 555900. DOI: 10.19080/JGWH.2019.14.555900
Benjamin DR, Frawley HC, Shields N, van de Water AT, Taylor NF. Relationship between diastasis of the rectus abdominis muscle (DRAM) and musculoskeletal dysfunctions, pain and quality of life: a systematic review. Physiotherapy. 2019 Mar 1;105(1):24-34.
Benjamin DR, Van de Water AT, Peiris CL. Effects of exercise on diastasis of the rectus abdominis muscle in the antenatal and postnatal periods: a systematic review. Physiotherapy. 2014 Mar 1;100(1):1-8.
Fernandes da Mota, P. G., Pascoal, A. G., Carita, A. I., & Bø, K. (2015). Prevalence and risk factors of diastasis recti abdominis from late pregnancy to 6 months postpartum, and relationship with lumbo-pelvic pain. Manual therapy, 20(1), 200–205. https://doi.org/10.1016/j.math.2014.09.002
Gluppe, S., Ellström Engh, M., & Kari, B. (2021). Women with diastasis recti abdominis might have weaker abdominal muscles and more abdominal pain, but no higher prevalence of pelvic floor disorders, low back and pelvic girdle pain than women without diastasis recti abdominis. Physiotherapy, 111, 57–65. https://doi.org/10.1016/j.physio.2021.01.008
Khandale SR, Hande D. Effects of abdominal exercises on reduction of diastasis recti in postnatal women. IJHSR. 2016;6(6):182-91.
Sperstad, J. B., Tennfjord, M. K., Hilde, G., Ellström-Engh, M., & Bø, K. (2016). Diastasis recti abdominis during pregnancy and 12 months after childbirth: prevalence, risk factors and report of lumbopelvic pain. British journal of sports medicine, 50(17), 1092–1096. https://doi.org/10.1136/bjsports-2016-096065
Van de Water AT, Benjamin DR. Measurement methods to assess diastasis of the rectus abdominis muscle (DRAM): a systematic review of their measurement properties and meta-analytic reliability generalisation. Manual therapy. 2016 Feb 1;21:41-53.
Wu, L., Gu, Y., Gu, Y., Wang, Y., Lu, X., Zhu, C., Lu, Z., & Xu, H. (2021). Diastasis recti abdominis in adult women based on abdominal computed tomography imaging: Prevalence, risk factors and its impact on life. Journal of clinical nursing, 30(3-4), 518–527. https://doi.org/10.1111/jocn.15568
Hickey, F., Finch, J.G. & Khanna, A. A systematic review on the outcomes of correction of diastasis of the recti. Hernia 15, 607–614 (2011). https://doi.org/10.1007/s10029-011-0839-4